Spinal conditions can range from mildly irritating to severely debilitating, making the prospect of spinal surgery a focal point for those seeking relief. The spine is an engineering marvel, composed of bones, joints, ligaments, and discs, all orchestrated to provide the body with a delicate balance of stability and flexibility. When this balance is disrupted by injury or disease, the impact on an individual’s quality of life can be profound. Surgery on the spine is performed to alleviate pain, restore function, and correct anatomical abnormalities. This blog delves into the common types of spinal surgeries, outlining the specific uses for each procedure and providing insight into when and why they might be necessary. With medical technology advancing rapidly, understanding these surgeries can offer hope and clarity to those navigating their spinal health journey.
Discectomy
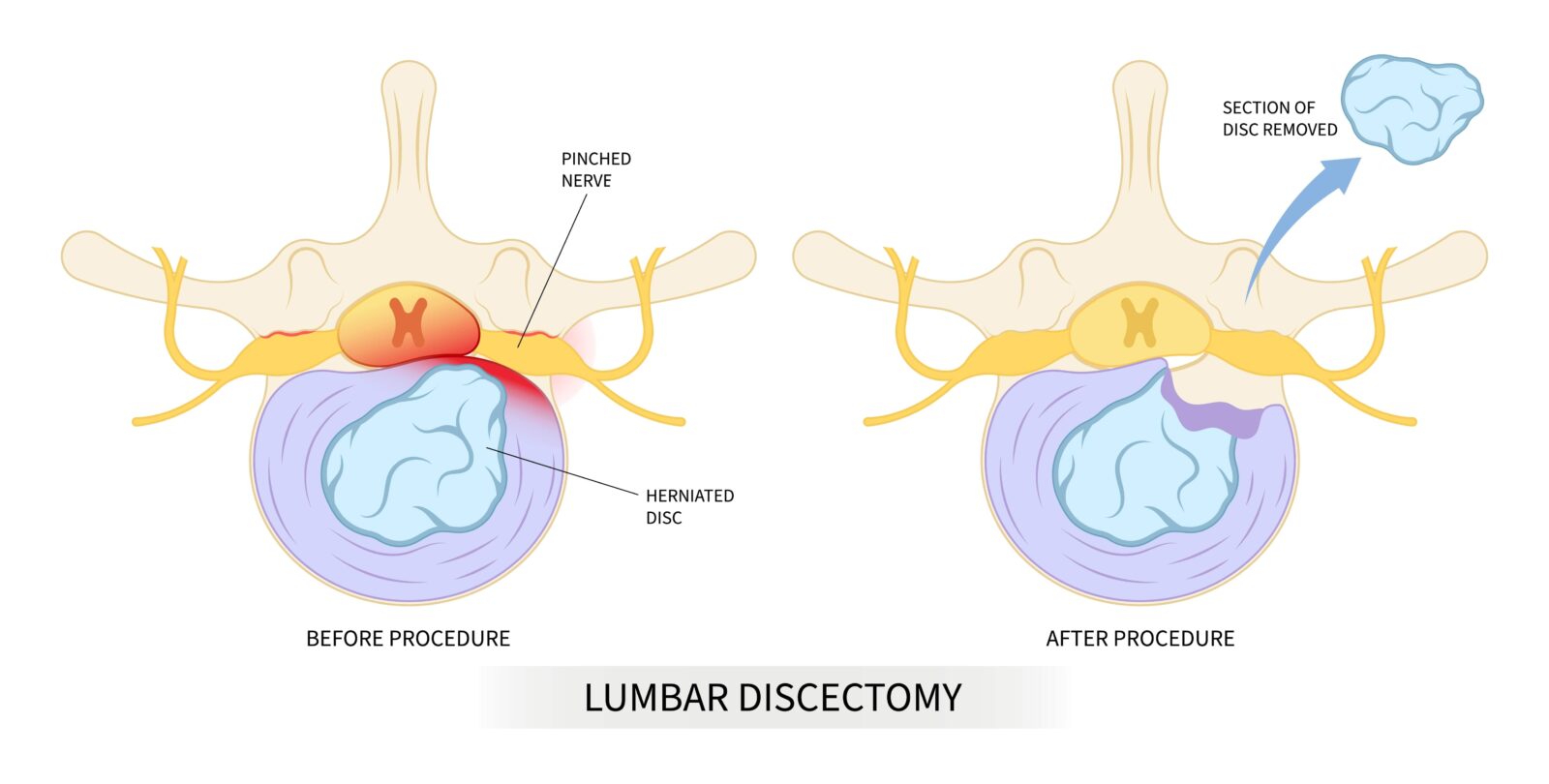
A discectomy is a surgical procedure to remove a damaged segment of a herniated disc in the spine, which can impinge on nerve roots or the spinal cord itself, causing intense pain, weakness, or numbness. Disc herniation occurs when the cushion-like pads between the vertebrae move out of position and press on adjacent spinal nerves. A discectomy is deemed necessary when conservative treatments such as physical therapy, medication, and spinal injections fail to provide relief, or when the patient experiences significant functional impairment or neurological deficits, such as altered reflexes, diminished strength, or loss of bowel or bladder control. The goal of a discectomy is to relieve nerve pressure and alleviate associated pain, restoring the patient’s mobility and quality of life. This surgery is one of the most common spinal procedures and has a high rate of success in relieving radicular pain or sciatica.
Laminectomy
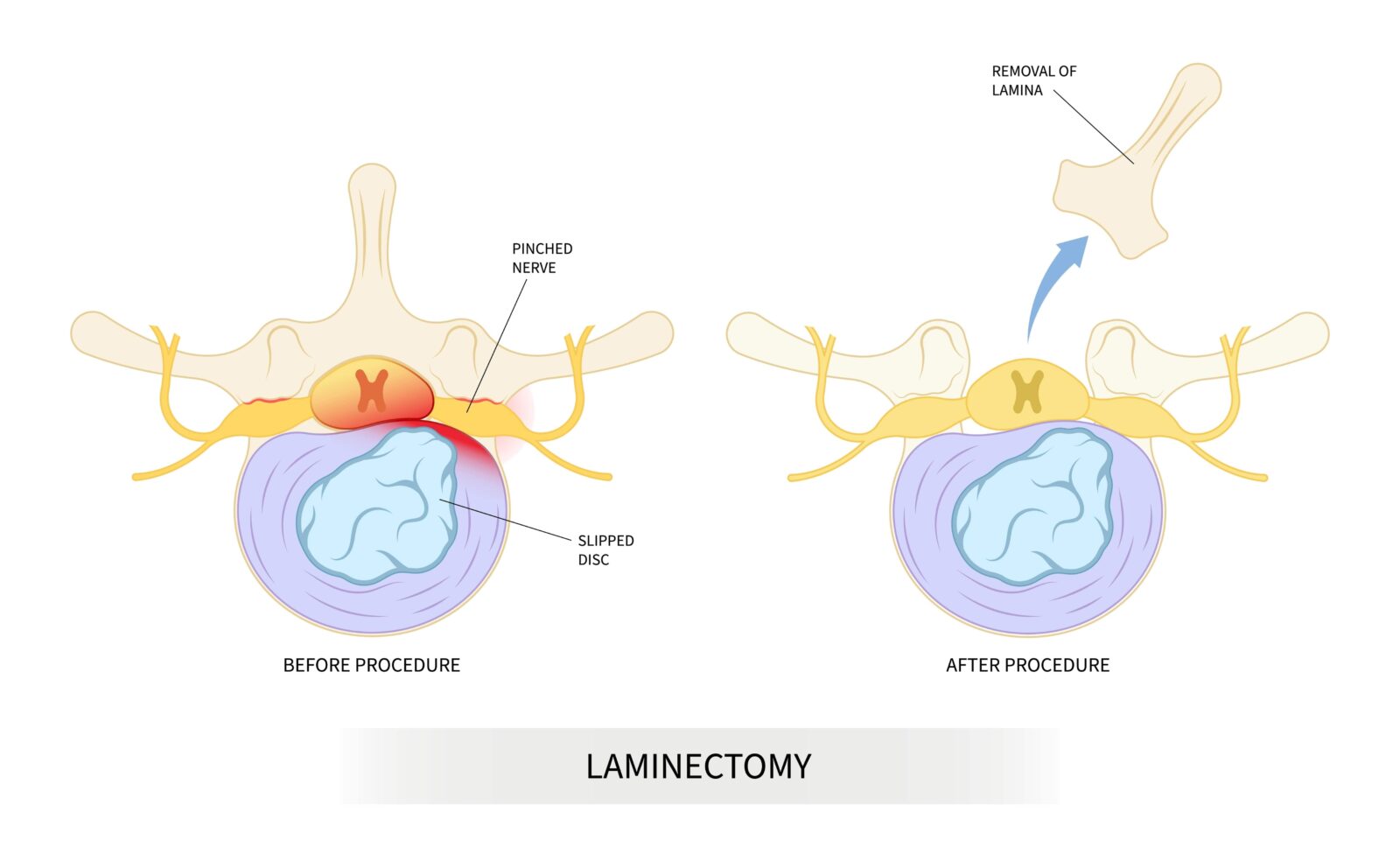
A laminectomy is a type of spinal surgery that involves the removal of the lamina, the rear portion of a vertebra covering the spinal canal, to create more space and relieve pressure on the spinal cord or nerve roots. This procedure is particularly effective in treating spinal stenosis, a condition that causes the narrowing of the spinal canal and results in pain, numbness, or weakness, typically in the legs or lower back. It may also be used to treat other conditions such as herniated discs, if they are contributing to the compression of nerve roots in conjunction with stenosis, and is also applied in the removal of tumors that press on spinal nerves. Laminectomy is recommended when more conservative treatments, such as physical therapy or medication, have failed to improve the patient’s condition, or when the patient experiences more severe or progressive symptoms like difficulty walking, loss of balance, or incontinence, which suggest that nerve compression may be leading to permanent nerve damage. The surgery aims to alleviate discomfort, restore function, and halt the progression of symptoms associated with these spinal conditions.
Spinal Fusion
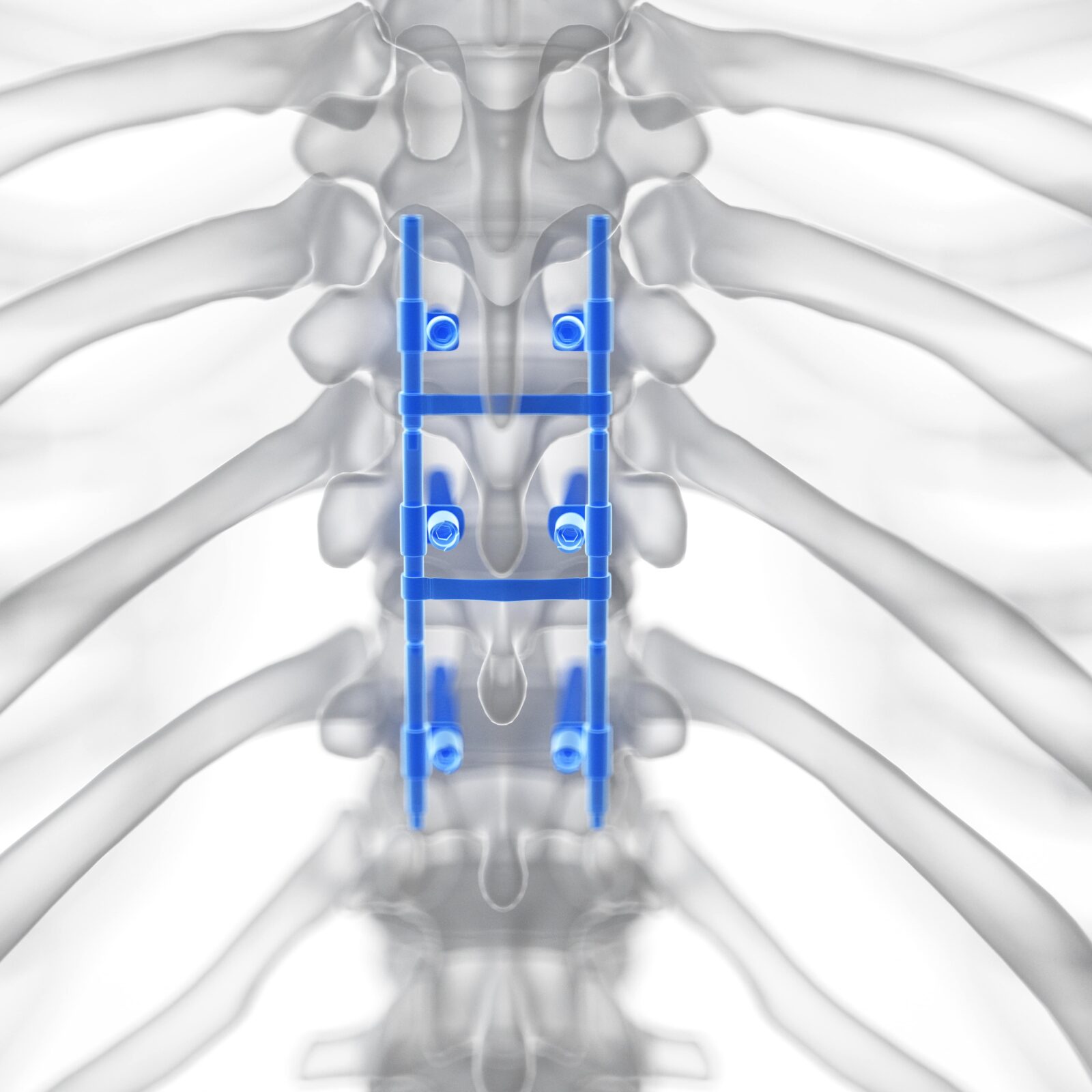
Spinal fusion is a surgical technique to join two or more vertebrae to prevent movement between them. Surgeons use bone grafts and hardware such as screws and rods to fuse the bones together permanently. This procedure is commonly used to treat a variety of painful spine conditions, including degenerative disc disease, spinal stenosis, scoliosis, fracture, infection, and tumor. By eliminating the movement of one or more spinal segments, fusion can significantly reduce pain caused by mechanical movement. Spinal fusion is recommended after other less invasive treatments have been exhausted without success, or when a patient’s condition is severe and potentially debilitating. The goal is to stabilize the spine and provide a rigid column that relieves pain by maintaining proper alignment and eliminating motion at a problematic vertebral segment. It’s crucial for patients considering this surgery to understand both the potential benefits and the implications, such as the recovery time and the change in spine mechanics post-surgery.
Foraminotomy
Foraminotomy is a surgical procedure that involves expanding the foramen—the bony opening in the spine where nerve roots exit and travel to other parts of the body. This surgery is designed to relieve the pressure and compression on nerves that are often caused by conditions such as foraminal stenosis, bulging or herniated discs, scar tissue, or excessive ligament growth. By trimming or removing bone and other tissue that may be constricting the foramen, a foraminotomy restores nerve function and relieves symptoms such as radiating nerve pain, weakness, and numbness. This procedure is typically recommended for patients who suffer from significant and persistent symptoms that have not responded to conservative treatment measures like physical therapy, medication, or spinal injections. Foraminotomy can be a preferred treatment for targeted relief of nerve impingement, offering a potentially less invasive alternative to more comprehensive spinal surgeries with a focus on preserving as much of the natural structure and function of the spine as possible.
Vertebroplasty and Kyphoplasty
Vertebroplasty and kyphoplasty are minimally invasive spinal surgeries designed to relieve pain and stabilize the spine following vertebral fractures, typically caused by osteoporosis, cancer, or traumatic injury. In vertebroplasty, a special bone cement is injected directly into the collapsed or damaged vertebrae to restore strength and shape to the bone. Kyphoplasty expands on this technique by first inserting a balloon into the vertebra and inflating it to create space, which is then filled with the bone cement, aiming to restore the original height and shape of the bone. Both procedures offer the benefit of pain relief and structural support. They are recommended for patients with acute vertebral compression fractures who experience severe pain that does not respond to conservative treatments, such as rest, pain medication, or bracing, or who suffer from related complications such as decreased mobility or spinal deformity. By stabilizing the fracture, these procedures can help reduce pain, prevent further collapse of the vertebra, and improve the patient’s functional abilities.
Artificial Disc Replacement
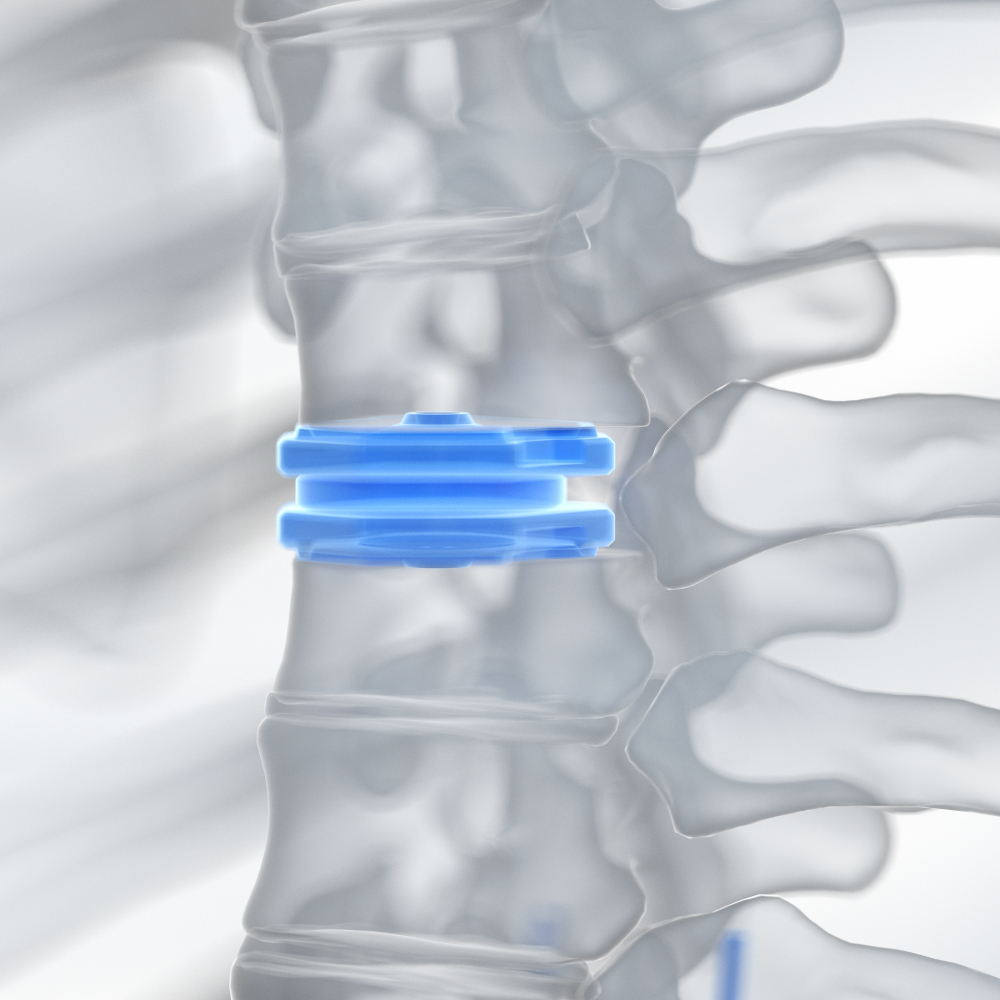
Artificial disc replacement is a type of spinal surgery where a diseased or damaged intervertebral disc is replaced with a prosthetic implant. This procedure is intended to mimic the form and function of the natural disc, preserving the mobility at the level of the spine after disc removal. It’s an alternative to spinal fusion for treating severe and chronic discogenic pain—pain originating from a spinal disc—often due to degenerative disc disease. The surgery may be beneficial for individuals with symptomatic disc problems that have not improved with extensive non-surgical care, such as physical therapy and medication. Ideal candidates are typically those without significant spine arthritis or deformity, who have maintained good spinal stability, and whose pain is localized to only one or two disc spaces in the spine. By replacing a worn disc, artificial disc replacement can alleviate pain while aiming to preserve more natural movement and reduce the stress on adjacent segments of the spine, potentially preventing further degeneration.
Conclusion
Spinal surgery is a field that has seen significant advancements, providing relief to many who suffer from debilitating spinal conditions. However, the complexity of the spine and its fundamental role in everyday movements makes the decision to undergo surgery significant. It is essential for patients to have detailed discussions with their healthcare providers to understand the full scope of their surgical options, the risks involved, and the postoperative care required for the best possible outcome.
With ongoing research and the development of newer, less invasive surgical techniques, the future for spinal treatment looks promising. Patients now have access to a wider range of options that come with the potential for less pain and faster recovery times, offering a renewed hope for those suffering from spinal conditions.











 in CA by O360®
in CA by O360®