Spinal conditions can cause significant pain and discomfort, affecting the quality of life for many individuals. Two common conditions that affect the spine are spinal osteoarthritis and degenerative disc disease. While they share some similarities, it is crucial to understand their differences to ensure accurate diagnosis and appropriate treatment. In this blog, we will explore and compare spinal osteoarthritis and degenerative disc disease in detail.
What is Spinal Osteoarthritis?
Spinal osteoarthritis, also known as facet joint arthritis, is a degenerative joint disease that affects the spinal joints. It is a common condition that occurs due to the breakdown of cartilage in the facet joints, which are located at the back of the spine where the vertebrae connect.

Cartilage is a smooth, slippery tissue that cushions the joints and allows them to move smoothly. In spinal osteoarthritis, the cartilage in the facet joints gradually wears away over time, leading to bone-on-bone contact and subsequent inflammation. This process can cause pain, stiffness, and decreased mobility in the affected joints.
Several factors contribute to the development of spinal osteoarthritis. Age is a significant factor, as the condition becomes more common with advancing age. Wear and tear over the years, repetitive stress on the spine, previous injuries, and genetic predisposition can also contribute to the development of spinal osteoarthritis.
The symptoms of spinal osteoarthritis can vary from person to person. Common symptoms include pain and stiffness in the affected area of the spine, which may worsen with movement or prolonged periods of inactivity. In some cases, spinal osteoarthritis can also cause radiating pain, tingling, or numbness into the arms or legs if the affected joints compress nearby nerves.
Spinal osteoarthritis is diagnosed through a comprehensive evaluation that includes a review of medical history, physical examination, and imaging tests like X-rays, MRI, or CT scans. Treatment aims to manage pain and improve joint function, often involving non-surgical approaches such as pain medications, physical therapy, exercise, lifestyle modifications, and assistive devices. In severe cases, surgical interventions like joint injections or fusion may be considered. Regular follow-ups and personalized treatment plans are essential for effective management of spinal osteoarthritis.
What is Degenerative Disc Disease?
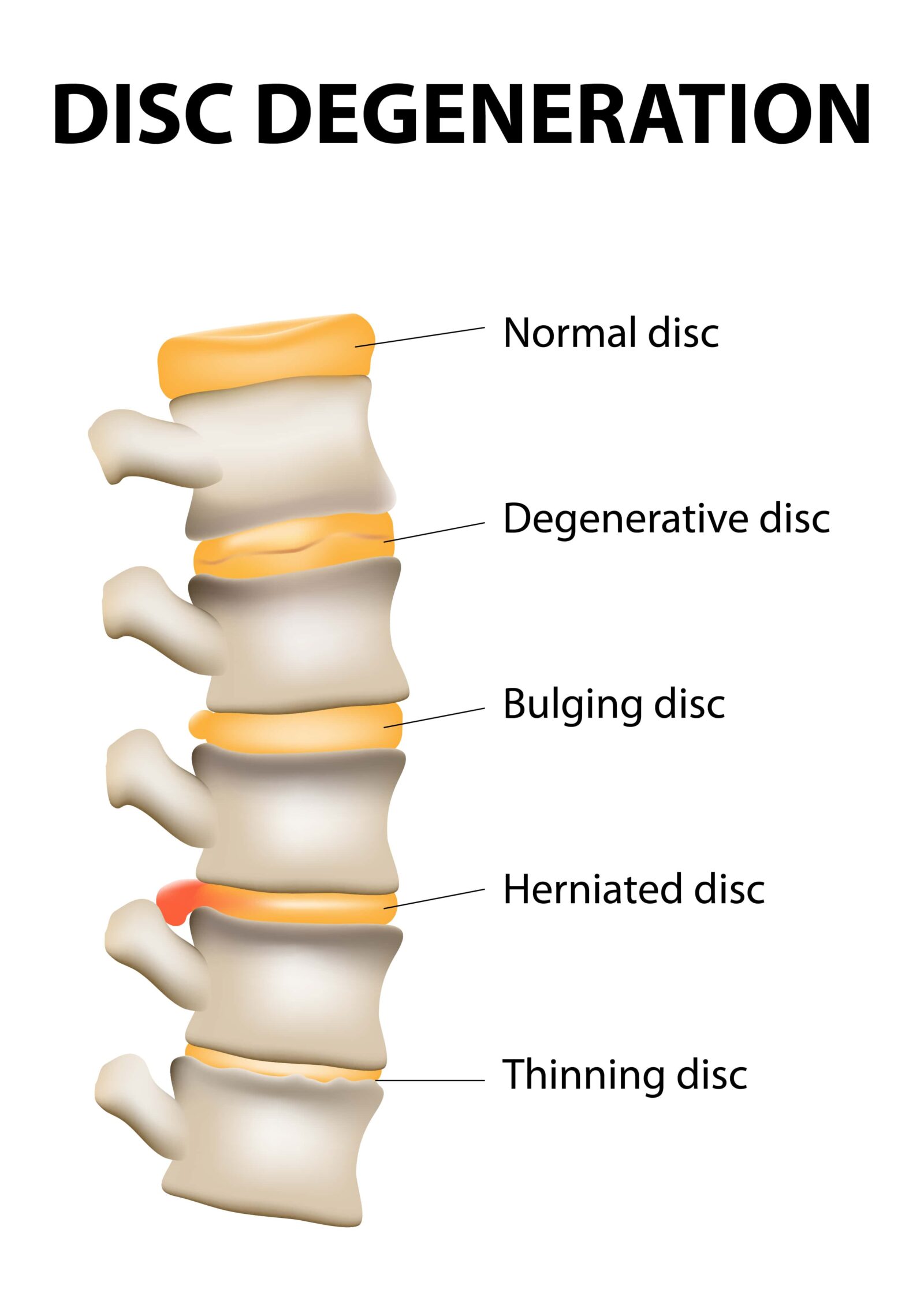
Degenerative disc disease is a condition that primarily affects the intervertebral discs, the soft cushions between the vertebrae of the spine. It is a common age-related condition where the discs undergo degenerative changes over time. The intervertebral discs serve as shock absorbers and allow flexibility in the spine. However, with degenerative disc disease, these discs gradually lose their water content and elasticity, leading to a reduction in height and compromised function.
Various factors contribute to the development of degenerative disc disease, including age, genetics, repetitive stress or injuries, and lifestyle choices. As the discs degenerate, they become less effective in absorbing and distributing forces during spinal movements. This can result in symptoms such as chronic low back pain, stiffness, muscle weakness, and, in some cases, radiating pain or numbness into the arms or legs if the degenerated discs compress nearby nerves.
Degenerative disc disease is diagnosed through a comprehensive evaluation that includes a review of medical history, physical examination, and imaging tests like X-rays, MRI, or CT scans. Treatment focuses on managing symptoms and improving quality of life, often involving non-surgical approaches such as pain medications, physical therapy, exercise, lifestyle modifications, and supportive devices. In severe cases or when conservative measures are ineffective, interventions like epidural steroid injections or surgical options such as discectomy or spinal fusion may be considered. Close collaboration with healthcare professionals and regular monitoring of symptoms are essential for effective management of degenerative disc disease.
Key Similarities Between Spinal Osteoarthritis and Degenerative Disc Disease:
Spinal osteoarthritis and degenerative disc disease share several similarities, including:
- Degenerative Nature: Both conditions are degenerative in nature, meaning they worsen over time. They are typically age-related and progress gradually as the affected structures undergo degenerative changes.
- Risk Factors and Demographics: Spinal osteoarthritis and degenerative disc disease share similar risk factors and affect similar demographic groups. Advanced age, genetic predisposition, repetitive stress or injuries to the spine, and certain lifestyle factors can contribute to the development of both conditions.
- Overlapping Symptoms: Spinal osteoarthritis and degenerative disc disease can have overlapping symptoms. These may include chronic low back pain, stiffness, limited range of motion, muscle weakness, and, in some cases, radiating pain or numbness into the arms or legs.
- Diagnostic Approaches: Both conditions are diagnosed using similar diagnostic approaches. Medical professionals rely on a combination of patient history, physical examination, and imaging tests such as X-rays, MRI, or CT scans to assess the condition of the affected structures and identify any associated abnormalities.
- Treatment Modalities: While the treatment approaches for spinal osteoarthritis and degenerative disc disease differ in some aspects, there are certain treatment modalities that may overlap. Both conditions often benefit from non-surgical approaches such as pain medications, physical therapy, exercise programs, and lifestyle modifications aimed at managing symptoms, improving function, and enhancing overall quality of life.
It is important to note that while spinal osteoarthritis and degenerative disc disease share similarities, they also have distinct characteristics and treatment considerations. Accurate diagnosis and individualized treatment plans are crucial to effectively address the specific needs of each condition.
Key Differences Between Spinal Osteoarthritis and Degenerative Disc Disease:
While spinal osteoarthritis and degenerative disc disease share similarities, it is crucial to understand their differences for accurate diagnosis and tailored treatment plans. Spinal osteoarthritis and degenerative disc disease have distinct differences, including:
- Affected Structures: The primary difference lies in the structures they affect. Spinal osteoarthritis primarily involves the facet joints, which are the joints located at the back of the spine where the vertebrae connect. In contrast, degenerative disc disease primarily affects the intervertebral discs, which are the soft cushions between the vertebrae.
- Underlying Mechanisms: Spinal osteoarthritis is primarily caused by the breakdown of cartilage in the facet joints, leading to inflammation and joint degeneration. Degenerative disc disease, on the other hand, is characterized by the degeneration of the intervertebral discs themselves, resulting in reduced disc height and compromised function.
- Predominant Symptoms: While there can be some overlap in symptoms, spinal osteoarthritis typically presents with localized pain, stiffness, and reduced range of motion in the affected joints. Degenerative disc disease often manifests as chronic low back pain, which may radiate into the buttocks, thighs, or lower legs. In some cases, it can also cause symptoms related to nerve compression, such as radiating pain, numbness, or weakness in the arms or legs.
- Imaging Findings and Diagnostic Criteria: The imaging findings and diagnostic criteria for spinal osteoarthritis and degenerative disc disease differ. Spinal osteoarthritis is typically characterized by the presence of bone spurs, joint space narrowing, and inflammation in the facet joints on imaging studies. Degenerative disc disease is diagnosed based on degenerative changes observed in the intervertebral discs, such as disc height loss, disc bulging, herniation, or the presence of Modic changes (bone marrow edema) near the discs.
- Treatment Approaches: Although there can be some overlap in treatment modalities, the specific treatment approaches for spinal osteoarthritis and degenerative disc disease may differ. Spinal osteoarthritis may benefit from interventions like joint injections or joint fusion surgery to alleviate pain and improve joint function. Degenerative disc disease treatment may focus on pain management, physical therapy, exercise, and techniques to maintain disc health, with surgical options like discectomy or spinal fusion considered for severe cases.
Understanding these differences is essential for accurate diagnosis and tailored treatment plans for individuals with spinal osteoarthritis or degenerative disc disease. Healthcare professionals can develop personalized approaches to address the specific needs and challenges associated with each condition.
In Conclusion:
Accurately diagnosing and distinguishing between spinal osteoarthritis and degenerative disc disease is essential for appropriate treatment and management. Understanding the differences and similarities between these conditions helps medical professionals develop individualized treatment plans for patients. If you are experiencing spinal pain or discomfort, it is important to seek professional medical advice for a proper evaluation. Ongoing research and advancements in the field of spinal disorders continue to provide hope for improved treatments and better quality of life for those affected by these conditions. In conclusion, spinal osteoarthritis and degenerative disc disease are distinct spinal conditions that require careful differentiation for effective treatment. By increasing our understanding of the differences between these conditions, we can improve diagnosis accuracy and optimize treatment strategies, ultimately leading to improved outcomes and enhanced quality of life for patients with spinal disorders.











 in CA by O360®
in CA by O360®