Spinal stenosis, a condition characterized by the narrowing of spaces within the spine, can cause significant discomfort and limitations for those affected. This condition often leads to pain, numbness, and muscle weakness, primarily when it compresses the nerves traveling through the spine. In this blog, we’ll delve into the nature of spinal stenosis and explore the surgical treatments available for this condition.
What is Spinal Stenosis?
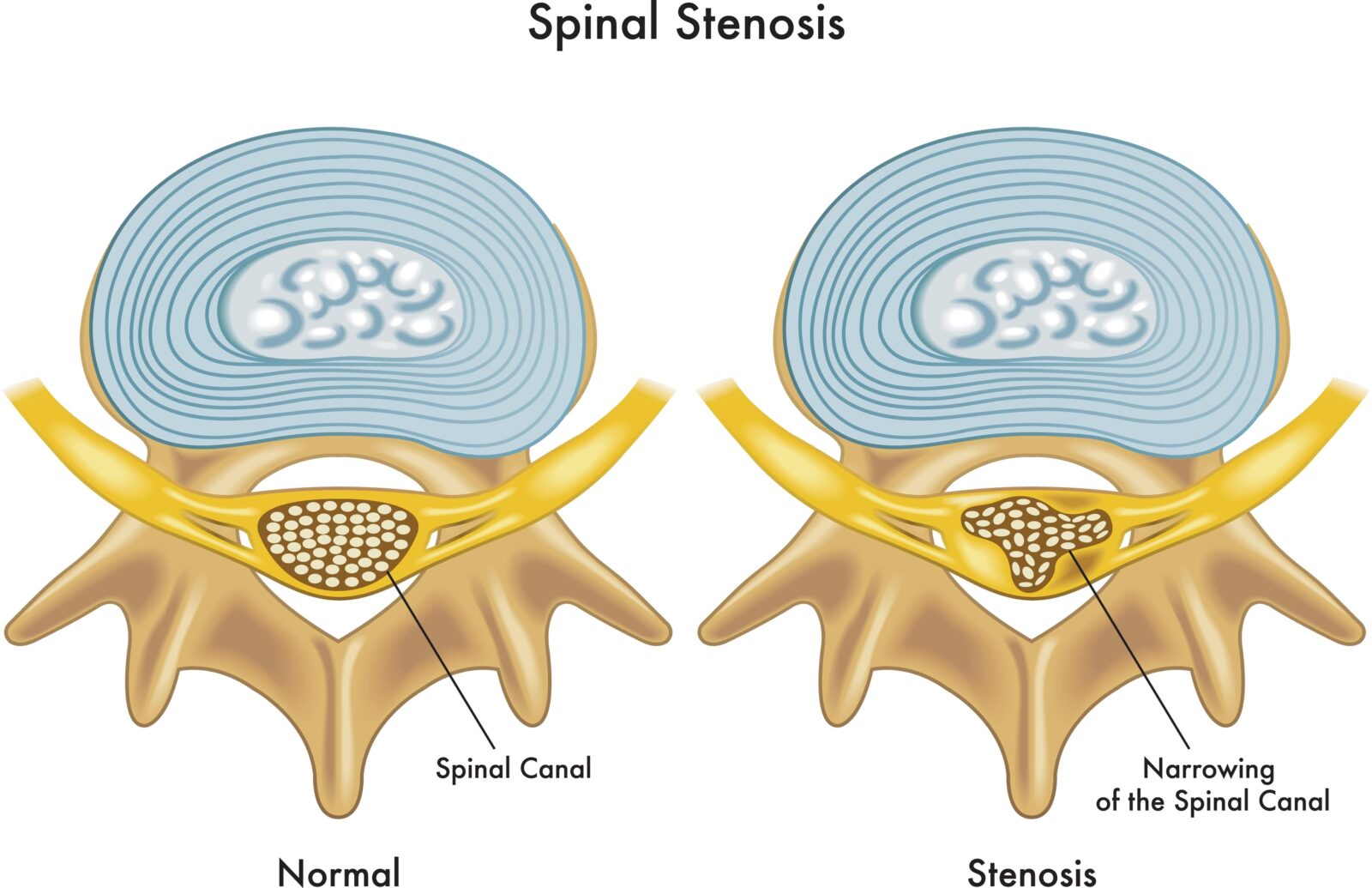
Spinal stenosis occurs when the spaces within your spine narrow, which can put pressure on the nerves that travel through the spine. It is most commonly caused by wear-and-tear changes in the spine related to osteoarthritis. In severe cases of spinal stenosis, doctors may recommend surgery to create additional space for the spinal cord or nerves.
Symptoms and Diagnosis
The symptoms of spinal stenosis can vary widely, but they often include:
- Pain in the back or neck
- Numbness, tingling, or weakness in the arms or legs
- Problems with balance
- In severe cases, bowel or bladder dysfunction
To diagnose spinal stenosis, healthcare providers typically perform a physical exam and may use imaging tests such as MRI or CT scans to get a clearer view of the spinal cord and the structures around it.
Surgical Treatments for Spinal Stenosis
When conservative treatments like physical therapy, medications, or injections fail to relieve symptoms, surgery may be considered. The goal of surgery is to relieve pressure on the spinal cord or nerves and maintain as much strength and flexibility in the spine as possible. Common surgical options include:
1. Laminectomy
This is the most common surgery for spinal stenosis. It involves removing the lamina (part of the bone that forms the vertebral arch in the spine) to create more space for the nerves. This procedure can sometimes cause the spine to become less stable, so the surgeon may also perform a spinal fusion at the same time.
2. Laminotomy
In this procedure, a surgeon removes only a portion of the lamina. This can relieve pressure on the nerve roots with less risk of destabilizing the spine compared to a laminectomy.
3. Foraminotomy
This surgery involves enlarging the foramen, the area where nerve roots exit the spine. By doing so, foraminotomy relieves pressure on nerves being compressed by herniated disks or bone spurs.
4. Spinal Fusion
During spinal fusion, two or more vertebrae are permanently connected. This procedure can help stabilize sections of the spine, but it reduces its flexibility.
5. Minimally Invasive Surgery
These techniques use smaller incisions and cause less damage to the surrounding tissues. They often result in quicker recovery times and less pain post-surgery.
6. Discectomy
A discectomy is performed to remove part of a herniated disc that is pressing on nerve roots or the spinal cord. While discectomy is primarily used for treating herniated discs, it can also be beneficial for patients with spinal stenosis when disc herniation contributes to nerve compression.
7. Anterior Disc Replacement
Anterior disc replacement is a newer surgical option that involves replacing a damaged disc with a synthetic one to maintain spinal mobility and relieve pressure on the spinal nerves or cord. This procedure can be an alternative to spinal fusion for certain patients, offering the advantage of preserving more natural movement in the spine.
Which Technique is Right for You?
The decision on which surgical technique to use for treating spinal stenosis is a complex one, involving several factors. Spinal surgeons consider a range of criteria to determine the most appropriate surgical approach for each individual patient. Here are the key factors that influence this decision-making process:
1. Severity and Location of Stenosis
The specific location and severity of the spinal stenosis play a crucial role in determining the surgical approach. For instance, if the stenosis is located in the lumbar spine and involves nerve root compression, a laminectomy or foraminotomy might be preferred. If a herniated disc is causing nerve compression, a discectomy may be the best option.
2. Overall Health and Age of the Patient
The patient’s overall health, age, and medical history are significant considerations. Younger, healthier patients might be better candidates for more invasive surgeries with longer recovery times, such as spinal fusion or disc replacement, due to their better ability to heal and tolerate surgery. In contrast, older patients or those with significant comorbidities might be steered towards less invasive procedures.
3. Presence of Other Spinal Issues
If the patient has other spinal conditions in addition to stenosis, such as degenerative disc disease or spondylolisthesis, the surgical approach may need to address these issues concurrently. For example, spinal fusion might be recommended to stabilize the spine in addition to relieving pressure caused by stenosis.
4. Symptomatology
The type and severity of symptoms also guide the choice of surgery. For patients with more severe or disabling symptoms, such as significant weakness, numbness, or pain that severely impacts their quality of life, more aggressive surgical interventions might be considered.
5. Previous Treatments
The surgeon will also consider what treatments the patient has already tried. For patients who have not found relief from conservative treatments, such as physical therapy, medications, or injections, surgery may be the next step. The type of surgery, however, will depend on the specific details of the patient’s condition and previous treatment responses.
6. Patient Preferences and Expectations
Patient preferences, expectations, and lifestyle are important factors in the decision-making process. Surgeons will discuss the potential benefits, risks, and recovery expectations of various surgical options with the patient to align on the best approach based on the patient’s goals and concerns.
7. Surgical Risks and Potential Outcomes
Finally, surgeons evaluate the potential risks and outcomes associated with each surgical option. This involves balancing the likelihood of symptom relief and improvement in quality of life against the risks of complications, recovery time, and the possibility of needing additional surgeries in the future.
Overall, the decision on the surgical technique for spinal stenosis is highly personalized. It requires careful evaluation of the patient’s specific situation, thorough discussion between the patient and surgeon, and a balanced consideration of all factors involved. This collaborative approach ensures that the chosen surgical method offers the best possible outcome for the patient’s unique case.
Risks and Considerations
Like any surgery, spinal stenosis surgery carries risks, including infection, nerve damage, blood clots, and anesthesia complications. It’s also important to have realistic expectations; while surgery can alleviate symptoms, it may not restore spinal function to the level it was before the onset of stenosis.
Post-surgery, patients often undergo rehabilitation, which may include physical therapy to help regain strength and flexibility. The recovery period can vary depending on the type of surgery and the individual’s overall health.
Conclusion
Surgical treatments for spinal stenosis can significantly improve the quality of life for those suffering from this condition. However, it’s crucial to thoroughly discuss the potential benefits and risks with a healthcare provider and consider all options. With proper treatment and care, many individuals with spinal stenosis can return to a more active and comfortable life.











 in CA by O360®
in CA by O360®