Cervical foraminotomy and discectomy are two surgical procedures that are commonly used to treat conditions that affect the cervical spine. While both procedures have similarities, they are also distinct in terms of the specific conditions they treat, surgical technique, and recovery time. In this blog, we will explore the differences between cervical foraminotomy and discectomy, as well as the factors to consider when choosing between the two procedures.
What is a cervical foraminotomy?
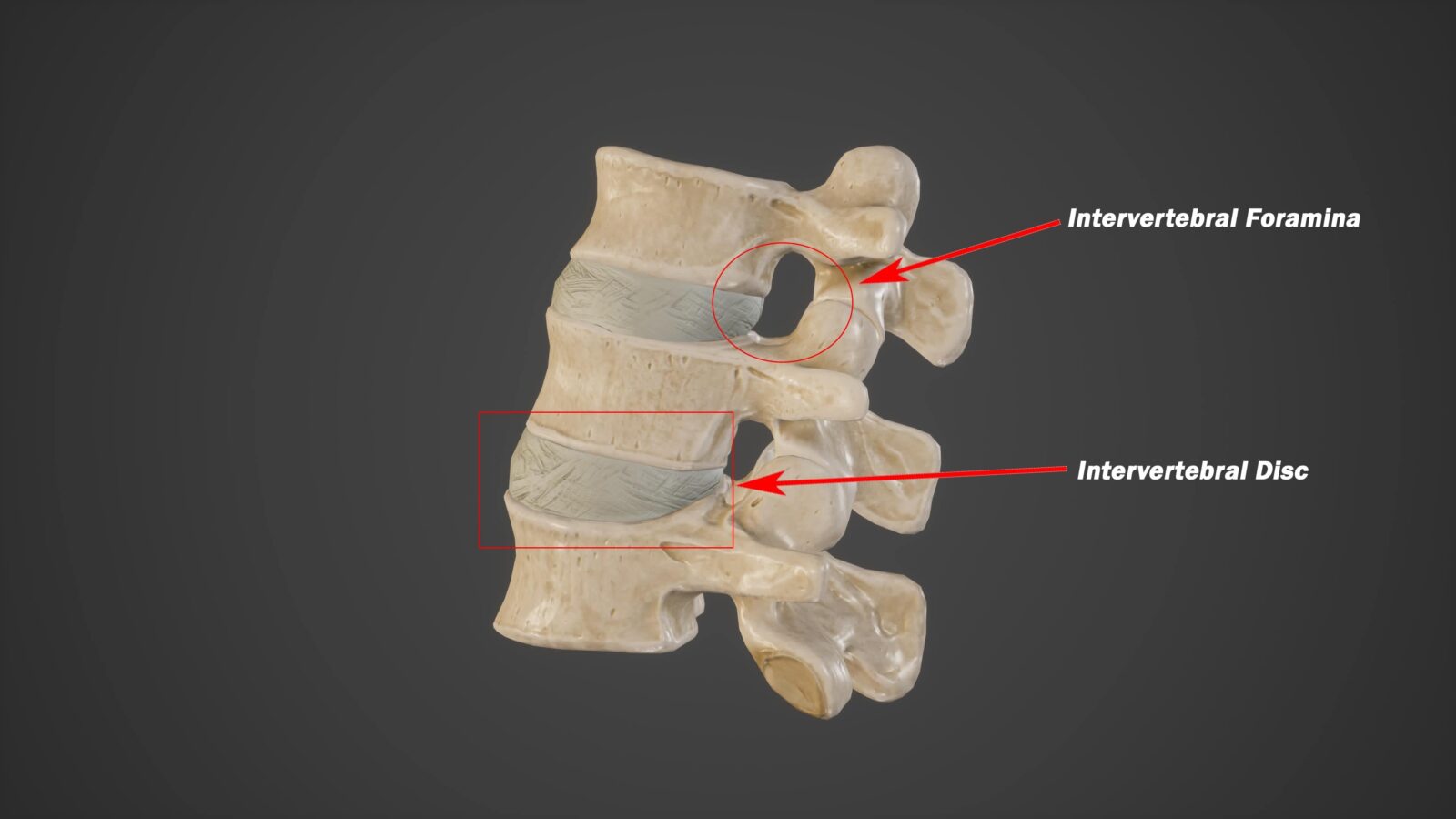
Cervical foraminotomy is a surgical procedure that is used to relieve pressure on the nerve roots that exit the spinal cord through small openings called foramina. The foramina are located on either side of each vertebra in the spine, and when they become narrowed due to injury or degenerative changes, they can compress the nerve roots and cause pain, weakness, and numbness in the arms, neck, and shoulders.
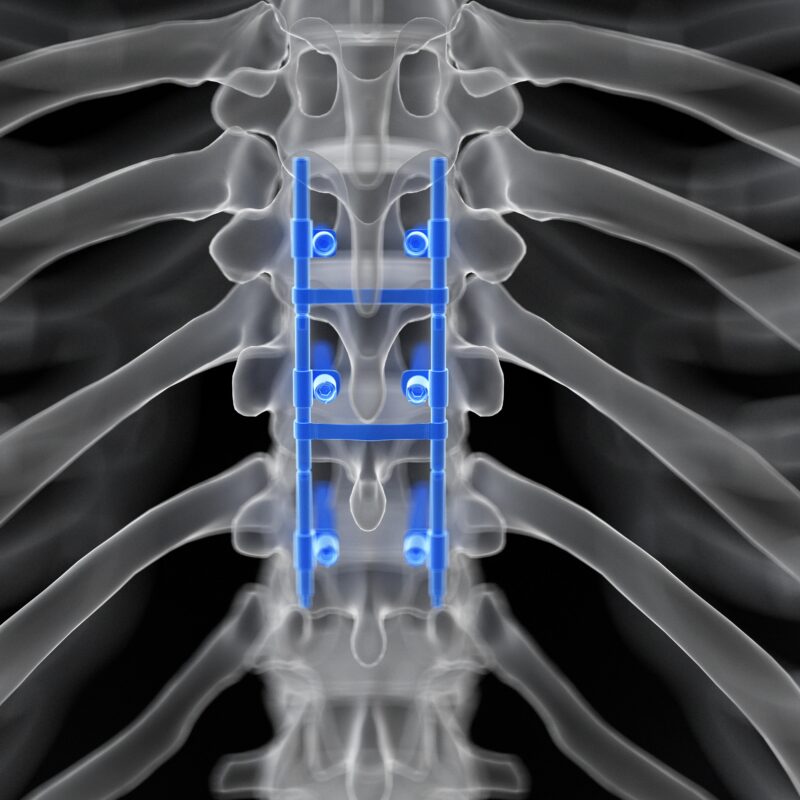
During a cervical foraminotomy, the surgeon makes a small incision in the back of the neck and removes a portion of the bone or tissue that is causing the compression of the nerve roots. This creates more space within the foramina, allowing the nerve roots to move freely and reducing pressure on them.
Cervical foraminotomy is typically used to treat a condition called cervical radiculopathy, which is caused by the compression of the nerve roots in the cervical spine. Cervical radiculopathy can result from a variety of conditions, including herniated discs, bone spurs, degenerative disc disease, and spinal stenosis.
Symptoms of cervical radiculopathy may include pain, weakness, and numbness in the neck, shoulders, arms, and hands. In some cases, patients may also experience tingling, burning, or a “pins and needles” sensation in these areas. The symptoms of cervical radiculopathy can range from mild to severe and can significantly impact a patient’s quality of life.
Cervical foraminotomy is typically recommended when more conservative treatments, such as physical therapy, medication, or steroid injections, have failed to provide relief. It is a relatively safe and effective procedure that can help to alleviate symptoms and improve mobility and function in patients with cervical radiculopathy. However, like any surgical procedure, it does carry some risks, and patients should discuss the potential benefits and risks with their surgeon before undergoing the procedure.
What is a cervical discectomy?
Cervical discectomy is a surgical procedure that is used to remove a damaged or herniated disc in the cervical spine. The cervical spine is the portion of the spine that is located in the neck, and it consists of seven vertebrae and six intervertebral discs that act as shock absorbers between the vertebrae.
During a cervical discectomy, the surgeon makes an incision in the front of the neck and removes the damaged or herniated disc. In some cases, a bone graft or artificial disc may be inserted to help maintain the normal spacing between the vertebrae.
Cervical discectomy is typically used to treat conditions such as cervical disc herniation, which occurs when the soft inner material of a disc bulges out through a tear in the tough outer layer and compresses the spinal cord or nerve roots. Cervical disc herniation can cause a range of symptoms, including neck pain, arm pain, numbness, tingling, and weakness.
Other conditions that may be treated with cervical discectomy include degenerative disc disease, which is characterized by the gradual breakdown of the intervertebral discs, and spinal stenosis, which occurs when the spinal canal becomes narrowed and compresses the spinal cord or nerve roots.
Cervical discectomy is typically recommended when more conservative treatments, such as physical therapy, medication, or steroid injections, have failed to provide relief. It is a safe and effective procedure that can help to alleviate symptoms and improve mobility and function in patients with cervical disc herniation or other cervical spine conditions.
Like any surgical procedure, cervical discectomy does carry some risks, including bleeding, infection, nerve damage, and spinal fluid leak. Patients should discuss the potential benefits and risks of the procedure with their surgeon before undergoing the surgery.
Key Differences
One of the primary differences between cervical foraminotomy and discectomy is the area of the spine that is targeted. Cervical foraminotomy is typically performed on the back of the neck, while cervical discectomy is typically performed on the front of the neck. Additionally, the specific conditions that are treated by each procedure differ, with cervical foraminotomy being used to treat cervical radiculopathy and cervical discectomy being used to treat cervical disc herniation.
Another key difference between cervical foraminotomy and discectomy is the surgical approach and techniques used. Cervical foraminotomy is a minimally invasive procedure that involves a smaller incision and less tissue disruption than cervical discectomy. Additionally, cervical foraminotomy is typically associated with a shorter recovery time than cervical discectomy.
Which procedure is best for you?
Choosing between a cervical foraminotomy and a cervical discectomy depends on several factors, including the underlying condition causing the symptoms, the extent of the spinal cord or nerve root compression, and the patient’s overall health and medical history.
In general, cervical foraminotomy is preferred for patients with nerve root compression caused by bony overgrowth or a herniated disc that is compressing the nerve root from the outside. The procedure is less invasive than cervical discectomy and typically involves a smaller incision, shorter surgery time, and faster recovery period.
On the other hand, cervical discectomy is recommended for patients with a more extensive herniated disc or spinal cord compression caused by a large disc herniation or degenerative changes in the disc. This procedure involves removing the entire disc and replacing it with a bone graft or artificial disc to restore the normal spacing between the vertebrae.
Ultimately, the decision between a cervical foraminotomy and a cervical discectomy should be made after a thorough evaluation by a qualified spine surgeon. The surgeon will take into account the patient’s symptoms, medical history, and imaging studies to determine the most appropriate surgical approach for the patient. Patients should also be aware that there are potential risks and complications associated with any surgical procedure, and they should discuss these with their surgeon before making a decision.
In Conclusion
In conclusion, cervical foraminotomy and discectomy are two distinct surgical procedures that are used to treat conditions that affect the cervical spine. While there are similarities between the two procedures, they differ in terms of the specific conditions they treat, surgical technique, and recovery time. Patients should work closely with their surgeon to determine which procedure is best suited to their individual needs and circumstances.